Why you should track insulin
The most trustworthy source of food and
fitness journalism in the country.
Editor’s note
I introduced the idea of ‘metabolic health’ — the health of the energy-generating and energy-processing apparatus inside our body — in this piece last year to set the frame for thinking about long-term fitness. Since then, we have published articles on managing blood glucose spikes, continuous glucose monitors and longevity. Today’s piece by Ankush Datar takes that forward by directing attention to an often ignored yet important biomarker: insulin. I learnt a lot from it, and am getting an insulin test next week!
Ankush is writing his debut book on health and wealth, set to be released in 2024. You can follow him on Twitter and or subscribe to his musings on Substack.
– Samarth Bansal
Jump to :
- What is insulin? Why does it matter
- What is ‘insulin resistance’?
- How it affects you
- How to measure insulin levels
- How to improve insulin sensitivity
Many of you might regularly get blood tests to check your blood sugar and cholesterol levels. And even if you are not, your doctor will ask you to get one following an illness. So you are in the know.
But there’s one crucial marker that often goes unnoticed, doesn’t get enough attention, and isn’t frequently recommended by doctors either. And that’s the marker which I think is among the most important ones to measure.
I am talking about insulin—the hormone that regulates blood sugar levels in our body. Insulin plays a vital role in converting sugar from the food we eat into energy, and its imbalance can lead to several health issues, from diabetes to heart disease.
Take my dad. He’s been managing diabetes for over thirty years, routinely monitoring his sugar levels. So when he asked me “Why do I need to take an insulin test?” I was astonished. Despite his high insulin levels and reliance on an insulin pen, he had never measured it himself.
Then there’s a friend of mine. She largely feels healthy, her blood sugar levels are normal, but her recent PCOS diagnosis revealed her insulin levels were abnormally high – a key factor contributing to her condition.
This lack of awareness about insulin’s importance is a common issue. Many don’t realise how crucial it is as a health metric, one that can help prevent chronic diseases in the long run. If prevention is better than cure, then tracking insulin is a step we shouldn’t overlook. And it’s important for everyone – not just those with existing health concerns.
Today’s piece is a primer on the significance of insulin. It’s also an argument for the action I strongly encourage you to consider: measuring insulin.
Let’s start with the basics.
1. What is insulin? Why does it matter?
Insulin is a hormone, a type of chemical messenger in your body, produced by the pancreas, an organ located behind your stomach. Its main job is to manage the sugar—glucose—in your blood.
Think of glucose as the fuel that your body’s cells need for energy. After you eat, your body breaks down the food into glucose, which enters your bloodstream. However, glucose can’t enter most of your body’s cells directly.
That’s where insulin comes in. It acts like a key, attaching to cells and ‘unlocking’ them, allowing glucose to enter from the bloodstream. This process lowers the amount of glucose in your blood.
Without this key, glucose remains in the bloodstream, leading to potential health problems like high blood sugar, energy imbalances, and over time, conditions like diabetes if not regulated properly.
2. What is ‘insulin resistance’?
Insulin resistance occurs when your body’s cells start responding poorly to insulin. This means your cells aren’t effectively taking in glucose.
In response, the pancreas begins producing more insulin to process this glucose. However, there’s a limit to how much it can compensate, and eventually, the pancreas may not be able to meet the demand. As a result, glucose levels can start to rise significantly.
The causes of insulin resistance are varied. It’s commonly linked to factors like being overweight or leading a sedentary lifestyle, but genetics and certain medical conditions also play a role.
Essentially, anything that hampers the body’s ability to use insulin effectively can lead to insulin resistance.
Why does this matter?
Because it’s about metabolic health. As Dr. Casey Means, the Chief Medical Officer and co-founder of metabolic health company Levels says:
“Insulin resistance is the root or key driver of almost every chronic disease in our society today, and knowing your fasting insulin is a key step in knowing where you stand. If it’s high, it’s a problem, and it’s straightforward to improve with diet and lifestyle.”
The message is clear: Paying attention to insulin is a precautionary measure for your health. It’s an early indicator.
Insulin resistance can precede Type 2 diabetes by 10 to 15 years—meaning early detection can provide a crucial opportunity for timely intervention to prevent its progression to Type 2 diabetes. And the risks aren’t limited to diabetes; heart disease and other conditions are also linked. In fact, it plays a hidden role in conditions like PCOS and affects overall health.
Many ask me if tracking blood glucose alone is sufficient. Is it?
Not exactly. If your blood sugar levels are abnormal, then yes, it indicates your insulin levels might be off. But the reverse isn’t always true.
Consider this scenario: Your pancreas is working overtime, producing lots of insulin to keep your blood sugar levels in check. Your blood sugar tests might seem normal, but they could be masking the underlying issue of insulin overproduction.
Which is why tracking both glucose and insulin offers a complete picture of metabolic health.
So, to sum up, what do we want? We aim to keep insulin levels low but within a healthy range. This ensures that insulin can effectively regulate blood sugar levels, maintaining a balance where they are neither too high nor too low. By achieving this balance, we can help prevent the onset of insulin resistance and its associated health complications, ensuring better overall metabolic health
Don’t resist sharing with your friends 🙆
3. How it affects you
Let me make the stakes more clear with specific, relatable examples:
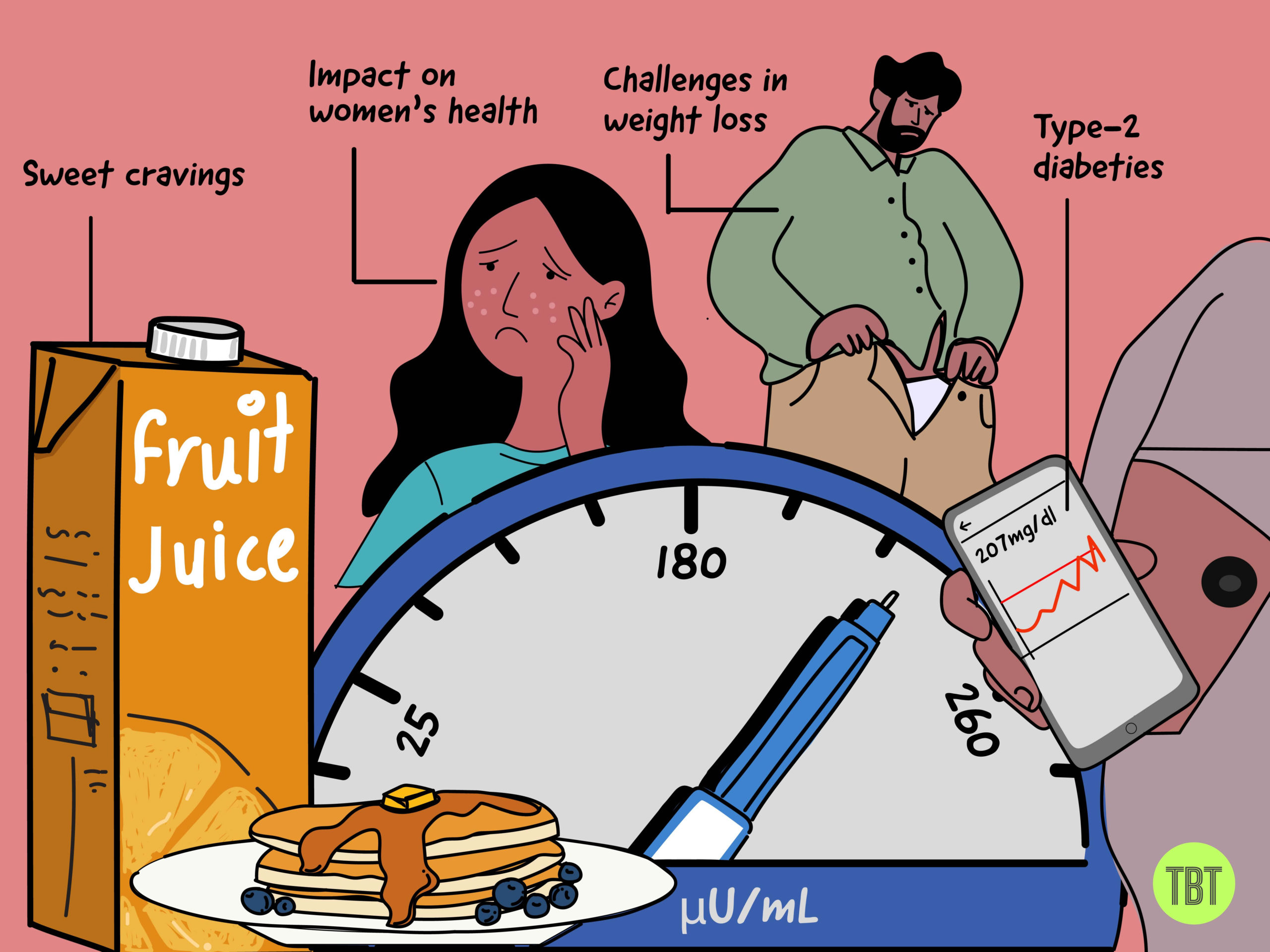
A) Hunger and eating habits: Ever find yourself feeling hungry soon after eating? When insulin levels are high, as in the case of insulin resistance, they can disrupt the normal signals of hunger and fullness. This can lead to increased hunger and cravings, particularly for carbs and sugary foods, making it challenging to stick to a healthy diet.
B) Challenges in fat loss: Struggling to lose weight despite dieting? Elevated insulin levels can make it more difficult to lose fat. Insulin promotes the storage of fat and inhibits its breakdown. So, when insulin levels are constantly high, your body is more likely to store fat rather than burn it for energy, which can hinder your weight loss efforts.
C) Impact on women’s health (PCOS): For women wondering why they might have irregular periods or acne, high insulin levels are often linked with PCOS. Insulin resistance can increase insulin levels, prompting the ovaries to produce more male hormones (androgens). This imbalance can lead to symptoms of PCOS, such as irregular menstrual cycles, acne, and excess hair growth.
D) The road to type-2 diabetes: Persistent high insulin levels can lead to insulin resistance, a precursor to type-2 diabetes. It’s like a warning sign that your body’s ability to manage blood sugar is compromised, paving the way for diabetes if not addressed.
4. How to measure insulin levels
Insulin levels are typically gauged through a blood test, which evaluates the concentration of insulin circulating in your bloodstream.
The most widely used test is the fasting insulin test. For this, you’ll need to fast, meaning no eating for 12 hours or more, before the test. A blood sample is then taken to measure your insulin level. This test is crucial for assessing your baseline insulin level in a fasting state.
What should your insulin level be? There isn’t a universally agreed-upon optimal level. However, Dr. Casey Means from Levels suggests that, based on advice from five of their advisors, “fasting insulin should stay below 10 μU/mL, and ideally between 2-6 μU/mL.”
(My fasting insulin over the last year has been around 5.50 μU/mL.)
In addition to the fasting test, doctors sometimes conduct a postprandial test — that is, after you eat — to observe how your body responds to food in terms of insulin production.
Know someone facing these symptoms? Share it them 🙂
5. How to improve insulin sensitivity
A) Change the order of your meals: veggies first, then protein and fats, carbohydrates at the end
- Begin with vegetables, which are high in fibre, which deploys itself on the wall of the upper intestine, forming a gooey mesh. This slows down digestion, causing a gradual, rather than rapid, increase in blood sugar.
- Incorporate proteins and fats next. They have minimal impact on blood sugar levels, helping to stabilise them. Plus, they make you feel full, and reduce your ability to binge on excessive carbs.
- Eat carbohydrates last. After your body has begun digesting the other nutrients, introducing carbs at this stage can help minimise overall blood sugar spikes, reducing the insulin response needed.
- A walk after eating, even if it’s just for 5-10 minutes, can significantly lower blood sugar levels. (Many realise this after using a CGM.)
- This helps your muscles use up glucose for energy, decreasing the amount in your bloodstream and reducing the need for additional insulin.
- Sleep is crucial for regulating hormones, including ghrelin (which increases hunger) and leptin (which signals fullness). Sufficient sleep ensures these hormones function properly.
- Lack of sleep disrupts this balance, often leading to increased hunger, overeating, and consequently higher blood sugar levels.
- Insulin assists in storing glucose in your liver and muscles. The liver can store a limited amount of glucose as glycogen, roughly equivalent to what’s found in two large McDonald’s fries.
- Muscles, however, can store much more glucose. Increasing muscle mass through strength training enhances this storage capacity.
- With more muscle mass, your body can store more glucose, reducing the need for excessive insulin production and preventing high blood sugar levels.

Go for an insulin test with a family member 🙂