I solved the mystery of the afternoon slump with CGM
Beat the afternoon slump with small tweaks
The most trustworthy source of food and
fitness journalism in the country.
Picture this: you’ve had a plate of aloo-puri for lunch. You sit down to work after your lunch break; suddenly, sleep seems unavoidable. The drowsiness feels like a drug—all you want to do is take a nap.
I’d felt this afternoon sluggishness for a long time but never understood why. Food is supposed to give me energy, so why do some meals slow me down?
I wanted to solve this mystery. I had one clue: it had to be about my metabolism—the biochemical process converting what we eat and drink into energy. And that led me to glucose, our body’s primary energy source. If I could somehow measure the impact of my diet on my body, I could crack the code.
And voilà, we have technology that makes it possible: a continuous glucose monitor or CGM, a coin-sized gizmo with a biosensor, usually applied on the back of the upper arm, with a small probe and a microneedle that tracks blood-sugar levels in real-time.
It’s like running a 24×7 lab test on your body that tells you how your choices impact your blood sugar levels.
Wearing a CGM for four months helped me learn what was right for my body. I made tangible changes in my everyday behaviour — changing the order in which I ate my food — after seeing real-time data. It made me understand how my dietary choices affected my energy levels and cognitive performance. And, of course, it helped me solve my afternoon slump problem. I will explain how.
Why was I specifically monitoring my glucose?
Now look, this technology is not new. CGMs were mainstreamed in the last two decades for managing diabetes, the chronic disease associated with consistently elevated blood sugar levels. However, it’s only in the past few years that adoption is extending to non-diabetic adults thanks to venture-funded health-tech startups.
In India, companies like Ultrahuman and Sugar.Fit sell software that adds an intelligence layer to the glucose data: the hardware (sensor) captures the glucose levels, and the software translates the raw stats into actionable insights. The algorithm suggests changes to optimise diet and workouts.
At the time I decided to invest in a CGM, I still didn’t fully understand how tracking blood glucose could be valuable for someone like me who did not have diabetes or prediabetes.
But I discovered a lot.
What do we want?
CGM shows a graph of glucose levels captured every minute.
You don’t want a spiky graph: big and frequent spikes (and crashes) indicate a problem. Yes, blood sugar will rise after most meals, and that’s fine—what you want is for the peak to be minimal and for glucose levels to quickly return to the baseline. (Do read our previous article on glucose to understand why.)
The optimal scenario is glucose levels staying in a healthy range for most of the day: between 70-120 mg/dl for approximately 90% of the day, says the US-based CGM company Levels.
I got my CGM from Ultrahuman, and their app tracks three key things: the time glucose levels stayed within the acceptable range, the fluctuation in glucose levels, and the average glucose levels over a period. These three metrics are combined to calculate a ‘metabolic score’ between 0 and 100.
The ideal reading is 80+, which is in the green range. The goal is to maintain or better this.
What I ate and how it affected me
Breakfast
I ate my breakfast on an empty stomach post a workout. I had a glass of coconut water, followed by a four-egg omelette and two homemade ghee-roast dosas. And boy, my glucose levels went through the roof.
So the next day I reduced the number of dosas to one to reduce my carbohydrate intake. No change. Glucose levels still spiked.
And then I changed the order in which I ate my food. I started with an omelette, took a five-minute pause, had a single dosa, and then coconut water.
Now the graph changed. Great glucose response. No spiky graph.
Why? Because protein and fats (in the omelette) help slow down carbs’ digestion and delay carbs’ absorption into the bloodstream.
This taught me a lesson I continue to follow: it’s not just about what you eat — the order in which you eat food matters.
More breakfast experiments: I replaced dosa with idli, poha, and upma. Same lesson:eat them, but the quantity of these high GI carbohydrates had to be checked to avoid higher-than-normal spikes.
The only standout was sabudana khichdi — even small quantities skyrocketed my glucose levels. (I left this for a day of indulgence.)
I started ensuring that I ate proteins and fats first, followed by carbohydrates. On days when I don’t workout, I stick to only proteins and fats. Structuring my morning kept me energetic, and I had high levels of cognition at work.
Now for lunch
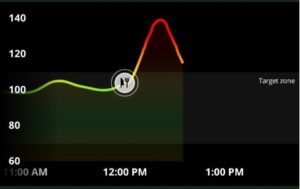
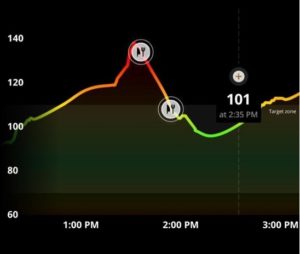
Come afternoon, and I found it difficult to keep my eyes open while reading at my work desk. I checked my CGM app and saw my blood glucose trend—my levels were elevated and stayed there.
I’d binged on carbs in the afternoon when my body did not require glucose. This spike and the eventual crash were the afternoon slump—I’d found my culprit.
I thought about the countless lunches where I had eaten more than the required quantity of rice or chapati and, on occasion, even had a bite of something sweet my colleague had offered. I’m sure you’re guilty of this too.
So, how could I prevent this from happening?
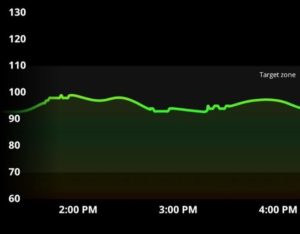
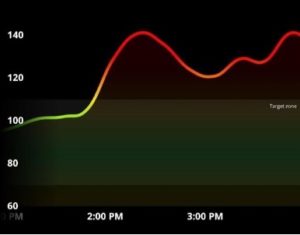
The above picture shows a good reading as my blood glucose response was controlled, and I was full of energy even after lunch with no issue of shut-eye. The key difference was having a meal with protein and adequate vegetables with high fibre content to slow down the glucose response.
Evening chai
The evening chai is the trickiest part of anyone’s day when we are tempted to reach out for a packet of biscuits or snacks.
We generally drink our tea or coffee along with our meals, but it is recommended to have your caffeine dose one hour before or after your meal as caffeine slows down digestion and can cause a short-term spike in blood glucose levels.
I observed that nuts—almonds, walnuts, and pistachios—produced a normal response. At times I accompanied this with a whey protein shake if I hadn’t met my protein requirements for the day. This combination produced a stable response.
Many of us eat fruits as a snack, but I do not eat fruits in isolation in the evening. When I do, I prefer eating kiwis, apples or bananas that are lower in sugar. I love watermelon and papaya but after seeing the glucose responses on my CGM, I controlled the quantities I have in a single sitting. The CGM showed me that my body does not react well to watermelon in higher dosages.
Fruits contain fructose, a naturally occurring sugar. So, although they are essential, the quantity we eat in a sitting or during the day needs to be checked. The conventional advice of eating a bowl of fruits at snack time could cause your glucose to skyrocket.
And finally, night-time arrived
My dinner includes the same protein I consume at lunch. I prepare two quantities simultaneously to ensure that my lunch and dinner are ready in one sitting. Along with this meal, I add complex carbohydrates with low GI, such as oats, sweet potato, or quinoa.
I buy steel-cut oats to avoid eating processed foods and mix them with flax, chia and pumpkin seeds to add flavour. Processed oats could cause higher-than-normal blood sugar spikes.
In my quest to solve the mystery of the afternoon slump, I also busted the myth that carbohydrates in the night are evil. Regulating your blood glucose throughout the day is imperative for a good night’s sleep and vice versa.
Moderate amounts of protein and controlled levels of carbs lead to a good sleep cycle. Studies have shown how high-protein diets can help adults sleep better. Tinkering and understanding how your blood glucose reacts to food and improving variability in your glucose level can eventually translate to good sleep, which leads to a positive cycle.
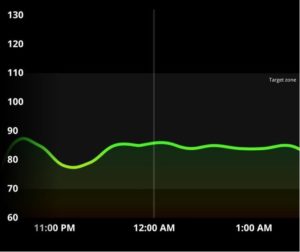
I occasionally drink too at night—vodka water with lime and salt. The reading above depicts a rosy image. However, each alcoholic drink has a different impact on your glucose levels based on the sugar content. I temper these effects by drinking water in between drinks.
But if you observed your CGM on a night when you’re drinking, the readings would shock you. Alcohol suppresses the glucose response which could also explain how you remain energetic on the dance floor with all that drinking. This blunting of glucose in your body is like a dormant volcano building up lava and erupting the following day.
Below is a picture of the day after drinking—I added a bit of quinoa to my lunch and saw a higher-than-normal spike. I figured that post a night of drinking, I must include a light workout and not eat too many carbs for better recovery.
What I learnt after monitoring my glucose
I started this experiment without knowing how a CGM could help someone like me. At the end of my time with the CGM, I was left with five takeaways:
1. Carbohydrates are not the enemy. Context is important—are you using carbohydrates for activity or recovery? If not, you can reduce the quantity of carbohydrates in your diet. Age, lifestyle, and pre-existing conditions play a huge role in how our bodies metabolize carbohydrates.
I tend to go zero carb at lunchtime. Here’s a simple way to gradually reduce your carb intake: reduce three chapatis to two chapatis; reduce a handful of rice to half-a-handful of rice and so on till you eliminate the carbs or keep them at minimal levels. Simultaneously increase the proportion of dal, chicken, paneer or soya that you consume at lunch. Take it slow.
2. Eat the fruit, avoid the fruit juice. Try this experiment with your CGM with orange juice—you will be surprised to see the massive difference in spikes between an orange and orange juice. Eating the whole fruit will also help control your calorie count.
3. Variation is important in what you eat and when you eat it. Proteins and fats with meals are crucial in developing good glucose variability. Changing the order in which I ate my carbs, proteins and fats improved my glucose response.
4. Exercise is key to maintaining an efficient metabolism, and some strength training should be mandatory in your protocol. A 10-minute walk after every meal can improve your glucose response to food and help you increase your step count.
5. Indulge, but moderation is key. When you want to indulge, don’t worry about glucose variations—just reduce the number of indulgences.
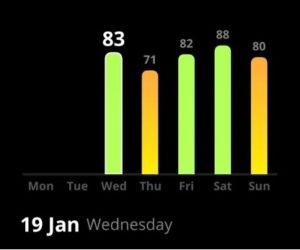
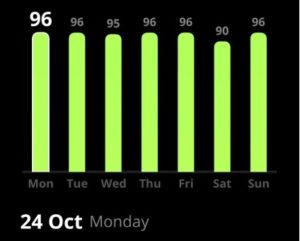
With the help of CGM, I could implement tweaks that improved my overall well-being, specifically suited for my body. The pictures above show the difference in my metabolic scores in one year. The scores are also a reflection of how I feel in terms of energy levels and cognition throughout the day as well as my athletic performance and sleep.
And I finally beat the afternoon slump.
Click the logo to sign up for the newsletter
More from Truth Be Told
Safest cooking utensils for healthy living
Your brain needs to relax and here’s how you can do it
Here’s how I got my cholesterol levels down
Why you can’t eat just one chip
The Definitive Guide to Smart Food Shopping
Eight swaps to eat better everyday
Diwali indulgence won’t make you fat
What spikes your blood glucose?
Is your body ageing gracefully?
Should you count calories?
Letters to Editor: Reader Response 01
My experiments with sleep
Why weight loss is a rigged game
You can’t be ‘healthy’, if you don’t know what it means
Food and fitness journalism is broken. We are fixing it.